Integrated Human Practices
Intro
Our original intention was to create a thermosensing patch for newborns that can be used when treating neonatal jaundice. However, we thought it was necessary to change the course of this project in that we received some negative feedback in an interview with a paediatrician. While seeking for a different application, we were conscious of the changes going on in our society due to the worldwide COVID-19 pandemic. And the one that caught our attention the most was the body temperature monitoring process at entrances of institutions.
At public facilities and institutions in Korea, body temperature is measured at the entrance with an infrared camera, and verification stickers are distributed to those who have normal body temperature. The problem is that since body temperature is checked only once upon entrance, continuous monitoring is impossible. Also, the current system is very vulnerable considering the possibility of malfunctioning of thermal cameras or temporary fluctuations of body temperature. We thought our Thermopatches could reinforce the monitoring system. By distributing our stickers to people entering the building, and requiring the stickers to be applied to the neck or wrist, continuous monitoring of body temperature would be made possible.
To evaluate whether this direction is worth pursuing, we interviewed one of the “gatekeeping” volunteers who monitor entrants’ body temperature at our institution. The interview proved that using Thermopatches for this application is worthy. Also, the feedback we received during the interview was very helpful in developing our concept of Thermopatches into an actual design and a user scenario.
Interview with a pediatrician : about jaundice patients.

A pediatrician’s thoughts about the application of our Thermopatch(RNA aptamer-based thermo-sensor) on monitoring body temperature of jaundice patients.
1. Why we interviewed:
Since our thermo-sensor requires an ambient light source of a certain wavelength, we thought that our would be suitable for jaundice patients receiving phototherapy. We intended to design our thermo sensors in a form of a sticker that can be applied to the patient’s skin. In case of a fever, our aptamers contained in the sticker will light up instantly. To evaluate whether our sticker suits this purpose, we consulted a pediatrician. (transcript shown below)
2. What we learned:
We obtained detailed information on symptoms and treatment of jaundice. Jaundice is a disease caused by accumulation of bilirubin in the infant patient’s body, especially threatening for premature infants. Treatment is done by exposing the patient to blue light at the incubator and usually infants are attached to a digital thermometer for monitoring body temperature. More importantly, we learned that our thermopatches are inferior compared to already commercially produced digital products in terms of accuracy and responsiveness. Also, various, rigorous requirements which medical appliances need to meet were too challenging for us to handle.
3. Results(how this interview affected our project):
After this interview, we decided to seek another suitable application which requires thermosensing. We eventually changed the course of our project and decided to apply our Thermopatches for monitoring fever symptoms of entrants to reinforce the current preventive measures for the spread of COVID-19.
Intro: Since our thermo-sensor requires an ambient light source of a certain wavelength, we thought that our would be suitable for jaundice patients receiving phototherapy. We intended to design our thermo sensors in a form of a sticker that can be applied to the patient’s skin. In case of a fever, our aptamers contained in the sticker will light up instantly. To evaluate whether our sticker suits this purpose, we consulted a pediatrician. (transcript shown below)
After this interview, we learned that our thermopatches are inferior compared to already commercially produced digital products in terms of accuracy and responsiveness. Also, various requirements which medical appliances need to meet were too challenging for us to handle. Thus, we decided to seek another suitable application which requires thermosensing.
Interview transcript
Interviewee: Jinhee Oh, Prof. of Department of Pediatrics, Catholic University of Korea, Seoul, Korea
Q1: First, could you briefly tell us about the symptoms of jaundice and how treatment is done?
A1: Jaundice is caused by accumulation of bilirubin in the infant patient’s body. Premature infants are more vulnerable to this disease since they don’t have a well-established BBB. They could experience choreoathetoid movement, a type of a seizure, and if they are left untreated, it could lead to irreversible neurological disorders. Visible symptoms include yellowness of the skin which can be diagnosed by a bilirubin sensor which measures how yellow the skin is. Though monitoring is crucial for infants, fever is not one of it’s symptoms.
Treatment is done by exposing the patient to blue light at the incubator. Since premature infants are vulnerable to the lowering of body temperature, they are attached to a digital thermometer which constantly monitors the infant’s body temperature.
Q2: Do you think our project is suitable for this purpose? Any advice on how our project should improve to suit this application?
A2: I think that the main problem is that, as mentioned before, there already is a reliable product that constantly monitors the infant’s body temperature. I think it would be very difficult for your project to replace digital thermometers simply because they are so advanced.
Monitoring body temperature is critical for premature infant patients. It is a matter of life and death. So, the most important thing is that your project has to be reliable. It must quickly and accurately light-up when abnormalities are detected. If this is not achievable, I rather recommend you to apply this project to mature infants since they are not as vulnerable as premature infants to variations in body temperature.
Korea University Staff at entries
1. what we interviewed:
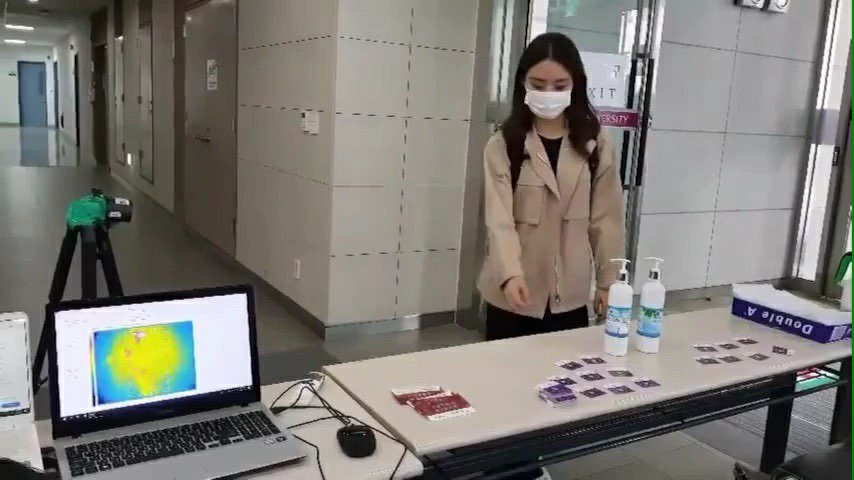
To get a detailed understanding on how our institution, Korea university, is responding to the pandemic, so that we could think about the improvements that could be made, we conducted an interview with the volunteers at our school. They are the ones in charge of monitoring entrants’ body temperature with thermal cameras and distribute ‘verification stickers’ if the visitor’s body temperature is within the normal range. This sticker, shown below, verifies that the individual has gone through the proper monitoring procedures our institution requires.
We requested the details of the current monitoring procedures, their thoughts on the possible flaws of the current system and their opinion on our project. The details of the interview are provided below.
2. what we learned:
We obtained a detailed description of the current monitoring procedures from the volunteer. It is worth noting his concern on the vulnerability of the current monitoring system. That provided, our project seemed meaningful in that it compensates the disadvantages of the current monitoring system. The interviewee’s opinion was that if we are able to come up with a functional product and a user scenario that specifies monitoring interval, Thremopatches are prospected to greatly enhance the reliability of the monitoring system
3. how we applied to our project:
It would be a better project if we devise the luminescence of stickers so that individuals can easily and instantaneously check them.
From this interview, we felt the necessity of a user scenario. The details of our user scenario are documented in the proposed implementation section.
To get a detailed understanding on how our institution, Korea university, is responding to the pandemic, so that we could think about the improvements that could be made, we conducted an interview with the volunteers at our school. They are the ones in charge of monitoring entrants’ body temperature with thermal cameras and distribute ‘verification stickers’ if the visitor’s body temperature is within the normal range. This sticker, shown below, verifies that the individual has gone through the proper monitoring procedures our institution requires.
We requested the details of the current monitoring procedures, their thoughts on the possible flaws of the current system and their opinion on our project. The details of the interview are provided below.
Q1. How does Korea University deal with the COVID-19 situation?
A1. Every student entering the building is stopped at the entrance and required to have their temperatures checked. We usually do it with infrared cameras. Students with temperature above 37.5℃ are set aside for a moment and are rechecked after 3-5 minutes, since it may be due to hot weather. We use a forehead thermometer the second time we check because forehead thermometers are considered more accurate than infrared cameras. If the measured temperature is still above 37.5℃, he or she isn’t permitted into the building and immediately asked to leave.
Q2. What are some problems with the current way of temperature checking?
A2. The biggest problem is inaccuracy and the lack of reliability of infrared cameras. Also, people’s normal body temperature varies on their own. With an infrared camera, the range is about 32~40℃. For these two reasons, we had to check people multiple times which is pretty inconvenient.
Q3. Do you feel that continuous observation of body temperature is necessary?
A3. It’s crucial to establish a definition of continuous monitoring regarding its interval and frequency. I sympathize with its strong necessity, but I think your team needs to get advice on monitoring intervals and periods from experts.
Q4. What is your opinion about our project?
A4. The existing thermal cameras are influenced by external factors such as heating due to the weather. In this context, body-attachable temperature measuring equipment will improve the accuracy significantly. If the luminescence of your stickers are detectable, your stickers could be more efficient and reliable in temperature monitoring than the current system.
Biosafety Interview with Professor Lee Sang-pal
1. Why we interviewed:
Based on the assumption that KUAS's project will actually be implemented, we conducted this interview to investigate the legal issues of Korea's Biosafety and take advice on this. Also, as the only university student team in Korea that participates in iGEM every year, we met Professor Lee Sang-pal to get advice on how to raise awareness of synthetic biology among the public and what KUAS can do for people who are not familiar with GMOs in Korea.
2. What we learned:
It seems that there is no big problem with the use of artificially synthesized genetic material such as DNA and RNA under the current bioethics and safety laws in Korea, but further consideration is needed because they may be provided for in other laws.
He also advised us that as university students, we should correct this and play a role in supporting communication through making video and card news to explain synthetic biology and molecular biology to the public easily.
3. How we applied to our project:
In order to communicate synthetic biology to the public following the professor's advice, we participated in "2020 Science Day" and communicated with people through video. We also created a card news that explains molecular biological knowledge in an easy-to-understand manner and uploaded it to KUAS' SNS account.
Biosafety's primary goal is to produce safe products that are not hazardous to human health and health care, and to ensure that laboratory researchers, developers and other related personnel are not exposed to danger during the production process of such products. In other words, the aim is to pursue comprehensive safety.
On Thursday, September 24th, 2020, we conducted an online meeting with Professor Lee Sang-pal of the Graduate School of Science and Technology Policy at Hanyang University on the theme of Biosafety. We briefed Professor Lee Sang-pal on our project and asked for advice on KUAS' activities.
The project uses artificially synthesized genetic materials such as RNA and DNA, but they do not seem to violate current bioethics or safety laws (although further consideration is needed because they may be provided for in other laws).
The Bioethics and Safety Acts prevents human and human materials from being researched, and prevents human dignity and value from being hazarded when dealing with embryonic genes. He said that human materials are defined as ”blood clots, plasma chromosome, DNA(Deoxyribonucleic acid), RNA(Ribonucleic acid), proteins, etc.”(Article2 of the Act). Instead, we received the opinion that in order to commercialize and use our project, we need to examine the laws on pharmaceutical safety in more detail (e.g., Act on testing and inspection in the food and drug industry and Regulation on drug safety, etc.).
He also said the Korean public is unfamiliar with molecular biology and needs to make efforts to raise social awareness. Regarding this, he advised that our KUAS team should correct this and play a role in supporting communication. We received an opinion that it is necessary to create videos with easy-to-understand knowledge of molecular biology, synthetic biology, and Biosafety, to improve the understanding and awareness of the general public through templates, and to share them on SNS. In the future, we thought that it would be necessary for our team to make an effort to actively provide the importance of molecular biology and sound information such as biosafety.

