Spinal Cord Injury Pathophysiology
Defining Spinal Cord Injury
Spinal cord injury (SCI) is the result of damage to the functional unit of the spinal cord - discs, vertebral bodies, posterior bony elements, posterior ligamentous complex and anterior and posterior longitudinal ligaments. SCI can be divided into three phases: acute, subacute and chronic. The acute phase encompasses the events that occur directly after the injury - vascular damage, ionic imbalance and necrotic cell death. It is then followed by the sub-acute phase, which involves apoptosis, demyelination of surviving axons, Wallerian degeneration and the evolution of a glial scar around the lesion. The chronic phase commences once neurorecovery plateaus and there is extension and enlargement of the glial scar, causing progressive axonal die-back and finally maturation of the glial scar (Alizadeh et al., 2019).
Clinical presentation after acute spinal cord injury depends on the type of spinal tracts affected and the extent of the injury. The American Spinal Injury Association impairment scale (ASIA), which is also used by the National Institute for the Health and Care Excellence (NICE) in the UK, enables initial classification following primary injury. (Kirshblum et al., 2011). The ASIA Impairment Scale (AIS) ranges from A-E, where A is the most severe and E is normal function in all segments following SCI. Damage to all tracts results in complete discontinuity and thus a complete injury, which is referred to as ASIA A injury; there is no sensorimotor function distal to the level of the lesion and no bladder or bowel (S4 and S5) function. Accordingly, it is sometimes described as “no Sacral Sparing injury” (Waters et al., 1991). Other injuries with an incomplete damage to sensory or motor tracts result in different clinical presentation patterns, depending on how many tracts are affected. Further classification of the different patterns of SCI is based on pattern of injury to primary tracts. It is vital to document injuries thoroughly to ensure the best treatment plan is devised (Rath and Balain, 2017).
We have decided to research into promoting axonal regrowth during the chronic phase as current therapeutic interventions tend to focus on prevention and mitigation of secondary injury in both the acute and subacute phase (Patek and Stewart, 2020). We have specifically targeted cervical spinal cord injuries in the chronic phase because of the formation of the cystic cavity at the site of the injury (also referred to as a syrinx); its pathogenesis is discussed below.
Defining Syringomyelia

Syringomyelia refers to the formation of an intramedullary cyst filled with cerebrospinal fluid (CSF) within the spinal cord, although its pathogenesis in patients with an associated spinal lesion is not completely understood (Heiss et al. 2012). Syringomyelia associated with spinal pathology is known as primary spinal syringomyelia (PSS) and it accounts for approximately one-sixth of all cases of syringomyelia. It may form as a consequence of traumatic injury, inflammation or compressive lesions that compromise the subarachnoid space. Other common types of syringomyelia include posttraumatic syringomyelia (PTS) and postinflammatory syringomyelia.
PTS manifests as progressive neurological deficit above the level of previous spinal cord injury that begins several months to years after initial trauma. Its incidence following the original trauma was estimated to be 1–4%, although with the availability of MRI the incidence appears to be much higher (Batzdorf, 1991). Postinflammatory syringomyelia results from a delayed reaction to meningitis, either infectious or chemical. Syringomyelia may also develop in association with compression of the CSF pathways by extramedullary tumors, osteophytes, or herniated intervertebral discs (Heiss et al. 2012).
As the cyst grows in size and extends through the damaged tissue, reduction in sensation and increased spasticity may be seen. However, in the case of PTS, the cyst has been shown to develop more rapidly. The onset of symptomatic PTS occurred earlier among patients with more advanced age, cervical or thoracic-level injuries, complete neurological injury at the index level, and fracture-dislocations, especially if patients underwent surgery for deformity correction and stabilization (Brodbelt and Stoodley, 2003).
Research papers discuss multiple hypotheses for the pathogenesis of syringomyelia (Elliott, 2009). To help clarify the distinction between each theory we reached out to Dr Novak Elliott who advised further investigation into the cranial-spinal pressure dissociation theory - it describes how a phase difference between the cerebrospinal fluid around the spinal cord and the vascular pressure in the small arteries of the spinal cord together can lead to the development of very small annular fluid connections. When these connections pump out of sync, it induces a dynamic one-way valve, which favours fluid being pumped into the spinal cord. The cyst forms due to the displacement of the cerebrospinal fluid that causes a pressure gradient between the intracranial space and spinal space. The pressure gradient promotes the enlargement and extension of the cyst and the increased epidural venous pressure together with CSF movement leads to structural weakness in the cord and ultimately to the cyst’s extension (Rai and Rai, 2015). The extension of the cyst during the chronic phase of the SCI further contributes to cell death and axonal inhibition (Burda et al. 2014) and coincides with maturation of the glial scar - a cavity created by the variety of CNS cells, including reactive astrocytes, microglia, fibroblasts, and Schwann cells. It develops as resident microglia, astroglia, and NG2-positive oligodendrocyte progenitor cells undergo reactive gliosis during the sub-acute stage of the injury. In their reactive form, glial cells are able to seal off injury epicentre, secreting various chemo repellents (such as semaphorin 3A and ephrins) and growth-inhibiting matrix components (tenascin and chondroitin sulfate proteoglycans) (Alizadeh et al., 2019). Glial scar has been identified as a major inhibitory factor to neuronal regeneration after traumatic injury to the CNS as it appears to prevent axonal sprouting and cell differentiation in subacute and chronic phases.
Spinal Cord Injury Pathophysiology
The mechanical damage to the local capillaries that accompanies the primary injury induces bleeding into the parenchyma - spinal cord tissue composed of gray and white matter - of the spinal cord. This potentially upregulates the release of cytokines and chemokines from astrocytes, macrophages and microglia and into the extracellular space, causing damage to the blood-spinal cord barrier and increasing its permeability. The accumulation of macrophages in the microenvironment further promotes expression of cytokines and chemokines, continuing the depletion of the barrier and inducing inflammation (Fan et al. 2018). Wallerian degeneration - active degeneration of the axons distal to the damaged neurons - accelerates the breakdown of cellular cytoskeleton and myelin. The resultant myelin debris accumulates, and when not cleared effectively, it promotes the infiltration of the damaged tissue by macrophages, which are able to cross the blood-brain barrier; this exacerbates chronic inflammation and prevents axon regeneration (Warden et al., 2001). Inflammation has a dual effect: although it helps tissue remodelling and clear debris of lesion it also creates more cytokines and other molecules that promote further tissue breakdown.
The physical damage to the spinal cord may also lead to neural tissue edema, which raises the interstitial pressure and compresses the surrounding blood vessels. This opposes the microenvironment of a healthy spinal cord where there is consistent blood perfusion, extensive vascular system, and a low number of inflammatory cells. Together, it prevents scar formation and eliminates any risk of oedema, lipid peroxidation and oxidative stress. In the healthy spinal cord, ionic homeostasis and no free radical-mediated damage ensures the protection of mitochondria membranes and the correct function of the transmembrane adenosine triphosphate-driven pump. The blood-brain barrier in the non-damaged spinal cord remains intact, preventing the entry of macrophages and development of chronic inflammation (Alizadeh et al, 2019; Fan et al. 2018).
SCI typically results in neuronal death by both necrosis and apoptosis. Necrosis occurs as a direct result of injury due to damage to neuronal cell bodies, whilst apoptosis - programmed cell death mechanism - can be caused by multiple factors including DNA damage, hypoxia, cellular stress and inflammation. During hypoxia, extracellular calcium ions move inside the cells, activating calcium-dependent proteases; this creates oxygen reactive species, leading to apoptosis. Cellular stress involves formation of oxygen free radicals and glutamatergic excitotoxicity - it can result from physical tear of the tissue, prompting cells to release their contents and therefore increasing neurotransmitter concentration in the environment; this means that cells keep having glutamate-powered bursts of activity, leading to toxicity. Excessive activation of glutamate receptors by excitatory amino acids leads to a number of deleterious consequences, including impairment of calcium buffering, further generation of free radicals, activation of the mitochondrial permeability transition and secondary excitotoxicity. Various types of cellular stress and exhaustion can lead to chromatolysis - an induced dissolution of the rough endoplasmic reticulum granules (known as Nissl bodies) - that occurs after cellular swelling and leads to neuronal death (Fan et al. 2018; Zhang et al. 2012).
As previously mentioned, the sub-acute and chronic phases of the spinal cord injury are often characterised by the formation and maturation of the glial scar, which sets both physical and chemical barriers to neuronal regeneration. Although in-vitro and in-vivo studies on the effects of surgical modulations of the glial scar on neuronal regeneration are limited, resection of the glial scar was advised by Dr Zin Khaing at the University of Washington in the case of the surgical insertion of our scaffolding. The cyst formed at the site of injury creates a barrier that blocks an interaction between the scaffold and the surrounding environment, therefore the resection of the lesion would create a more manageable glial scar. However, the decision whether to perform the resection needs to depend on the nature, severity and time of cord injury - it has been shown to significantly worsen functional recovery after a moderate contusion injury in rats and penetrative injury, possibly due to variable function of the glial scar based on the injury mechanism (Rasouli et al., 2009). Glial scars have been widely shown to limit the manifestations of the injury to the initial site of trauma, preventing further neuroinflammation and providing biochemical protection to the spinal cord. This particular function appeared to be less crucial in the case of hemisected SCI (where damage occurs to only one half of the spinal cord), therefore subsequent glial scar resection in such models has been shown to have a significant benefit.

Axon Regeneration Post SCI
The main difference between the axons of the central nervous system and those of the peripheral nervous system (PNS) is found in their ability to regenerate post-injury. CNS axons are unable to regenerate due to the unfavorable environment that surrounds them, with myelin-associated inhibitors and chondroitin sulfate proteoglycans being some examples of major inhibitors. The sprouting of injured axons represents an additional disadvantage to functional improvements of the lesioned area (Huebner and Strittmatter, 2009).
The inability to assure axon regeneration provokes additional hostile conditions on the recovery of the patient. If the re-growth of the transected axons doesn’t occur, the patient will not be able to regain complete functionality, as the signal will not be able to cross the injury site and spread to the rest of the body. The incorporation of the scaffold into the injured area will allow the creation of an environment in which axonal regeneration can occur, with anisotropic features mimicking the topography of the non-lesioned spinal cord (Hoffman-Kim et al., 2010).
A series of anisotropic cues will be used to provide axonal guidance as it has been demonstrated that guidance channels, such as pores, are crucial for axonal regeneration. This is essential because axons tend to grow in an unarranged manner, typically missing their target (Hoffman-Kim et al., 2010; Zhu et al., 2018).
Comparing Novel Approaches
Table 1: Comparing the novel approaches we considered in treating SCI.
| Hydrogel | Biocompatible Scaffolding | Protease | |
|---|---|---|---|
| What phase of SCI does it best target? | Hydrogels are primarily designed to target the acute phase of spinal cord injuries (Hong et al., 2017). | Scaffoldings are more successful in the treatment of the chronic phase (Tsintou et al., 2015). | Proteases, such as ChABC, can directly target the glial scar formed at the chronic phase of SCI (Bradbury et al., 2002). |
| Successfully promotes axonal regrowth? | Synthetic non-degradable hydrogels (modified and/or seeded with different cell types): yes in early phase of SCI. Cannot promote axonal ingrowth long term. Natural Injectable materials: yes but combinatorial approach needed (Kubinová et al., 2020). | PCL provided physical support for axonal regeneration (Wang et al., 2020). | ChABC treatment can aid in regeneration of lesioned axons, improve connectivity of surrounding intact pathways and act as a neuroprotector of injured projection neurons.Treatment to increase PP2A activity promotes neurite outgrowth and counteracts the inhibitory effect of CSPGs and MAGs. |
| Degradation Rate? | Resorbable hydrogels can degrade whilst stable hydrogels cannot. Exact degradation rate varies with different hydrogel materials. (Perale et al. 2011). | Our PCL scaffolding of initial molecular weight 60kDa, can degrade over 3-3.5 years, which is based on our simulations using parameter values from Hoque et al, 2012. | ChABCs are thermally sensitive and become partially inactive within the first week. |
| Is it adapted to the spinal cord’s geometry? | Limited scope in embodying pre-designed geometries due to their limited ability in incorporating complex design strategies (Billiet et al., 2012). | Scaffoldings require a fully characterised internal architecture, that matches the mechanical properties of the spine, which allows for a more personal treatment. Additionally, properties are easily manageable depending on how the user chooses to print their material. | The use of proteases to degrade the Syringomyelia in spinal cord injuries could stimulate the regrowth of axons, yet there is insufficient data on its effects on axon growth alignment. Without the additional support of nerve guidance channels or scaffold structures, axons do not seem to migrate back towards their targets. |
| Potential for Drug Delivery? | Hydrogels can easily include a drug delivery system. | Scaffolds made of certain biomaterials can include a drug delivery system. | Proteases can be delivered via intrathecal injection. Combination therapy with a drug is potentially possible but needs to be validated. |
| How Invasive? | Hydrogels can be administered via an injection, providing a minimally invasive solution when compared to surgical options. | The implementation of the scaffold is invasive, requiring surgical implementation to insert the scaffold. Only one surgery is required as the scaffold is biodegradable and resorbable and hence does not need to be removed. | Proteases can be administered via an injection, providing a minimally invasive solution when compared to surgical options. |
| Does it reduce the cavity size of the lesion? | Hydrogel supports axon growth within and around the cystic lesions in contusive SCI models but did not reduce cavity size (Hong et al., 2017). | The design of an open path with core scaffold did reduce the cavity size of the lesion. | ChABC reduced glial scar formation. (Lee et al 2015). Reduced astrogliosis and cavity formation were seen in a study that used a PP2A agonist to activate PP2A (Cheng et al. 2015). |
After preliminary research, it was concluded that our scaffold design provided a more comprehensive approach to treating spinal cord injuries. Below, we discuss the use of proteases in comparison to our scaffold and present our final deliberations in our evaluation.
Evaluating the Use of Proteases to Treat SCI
Growth inhibitory and matrix inhibitory molecules that are found within the fluid-filled cyst during the chronic phase of SCI create an inhibitory environment for neurite outgrowth, hindering neuronal regeneration following SCI. Recent research has identified that proteases - enzymes that catalyse protein breakdown - can be clinically useful in the treatment of syringomyelia. Protein phosphatase type 2A (PP2A) and Chondroitinase ABC (ChABC) have shown the most promising results. Thus, this report aims to compare the clinical efficacy of ChABC and PP2A, prior to comparing the more clinically effective treatment to the use of a scaffold for treating spinal cord injury.
What is Chondroitinase ABC (ChABC)?
Chondroitinase ABC can be purified from Proteus vulgaris by cation exchange chromatography. This enzyme catalyzes the removal of Chondroitin Sulfate side chains of proteoglycans. It is highly selective for the long linear polysaccharide side chain galactosaminoglycan (GAG), so it does not act on core proteins. This is vital for inhibiting CSPGs interactions with its receptor as CSPGs are potent inhibitors of neurite outgrowth and may play a key role in preventing regeneration following spinal cord injury (Burke and Yip, 2017).
How can ChABC be used for SCI treatment?
CSPGs are massively up-regulated after injury to the central nervous system and are highly expressed in the resultant glial scar. Glial scars are typically poor promoters of neurite growth but when treated with ChABC they become growth permissive. Pre-clinical evidence demonstrates beneficial effects of ChABC treatment following spinal cord injury; by expressing ChABC, we may be able to liberate CS-GAG chains of the CSPG core protein, which would prevent CSPG–matrix glycoprotein interactions.
Overall, ChABC treatment can aid in regeneration of lesioned axons, improve connectivity of surrounding intact pathways and act as a neuroprotector of injured projection neurons (Bradbury and Carter, 2011).
How can ChABC be delivered to the site of injury?
Currently, ChABC has been administered via intrathecal injection after being stabilised by trehalose at 37°C in clinical trials. Trehalose is needed due to the fact that ChABC is thermally sensitive and almost all of its enzymatic activity is lost within 3-5 days at 37°C and for ChABC to degrade CSPG-associated gluosaminoglycans a fresh supply would be needed at least every 2 weeks (Chau et al., 2004).
Trehalose ChABC (TS-ChABC) delivered by a lipid microtube-hydrogel scaffold system was shown to be enzymatically active for at least 2 weeks in vitro and resulted in low levels of CSPG for 6 weeks after an in vivo delivery. It was also demonstrated that TS-ChABC hydrogel-microtube delivery system can be a more efficient alternative to the chronically implanted pumps typically used to deliver ChABC in vivo. This approach does not only make the delivery of ChABC less invasive but also allows the additional use of neurotrophic factors (Lee et al., 2010).
Are there any limitations of ChABC treatment?
While trehalose ChABC treatment was shown to be successful, the molecular mechanism of trehalose-mediated thermostabilization is poorly understood. There are several hypotheses outlining the mechanisms of protein stabilization by trehalose, including water replacement, preferential hydration, vitrification of solutions, and the influence of trehalose on the water–tetrahedral hydrogen bond network (Hédoux et al., 2009).
The diffusion of ChABC into deep regions of the spinal cord, when delivered via an intrathecal injection, is limited due to the large size of the enzyme and the overflow beyond the intrathecal space and attendant dilution. This means that multiple applications are required for efficacy, which may increase the risk of infection and further damage (Day et al., 2020). This limitation can be potentially overcome by a gene therapy approach of enzyme delivery - changes to the bacterial gene that are required for the bacterial enzyme secretion by mammalian cells were identified, and the efficacy of this method and vector delivery was successfully tested on a rat model of SCI (Bartus et al., 2014).
Negative side effects of the treatment include aberrant sprouting and aberrant plasticity, the latter of which leads to neuropathic pain (Woolf and Salter, 2000).
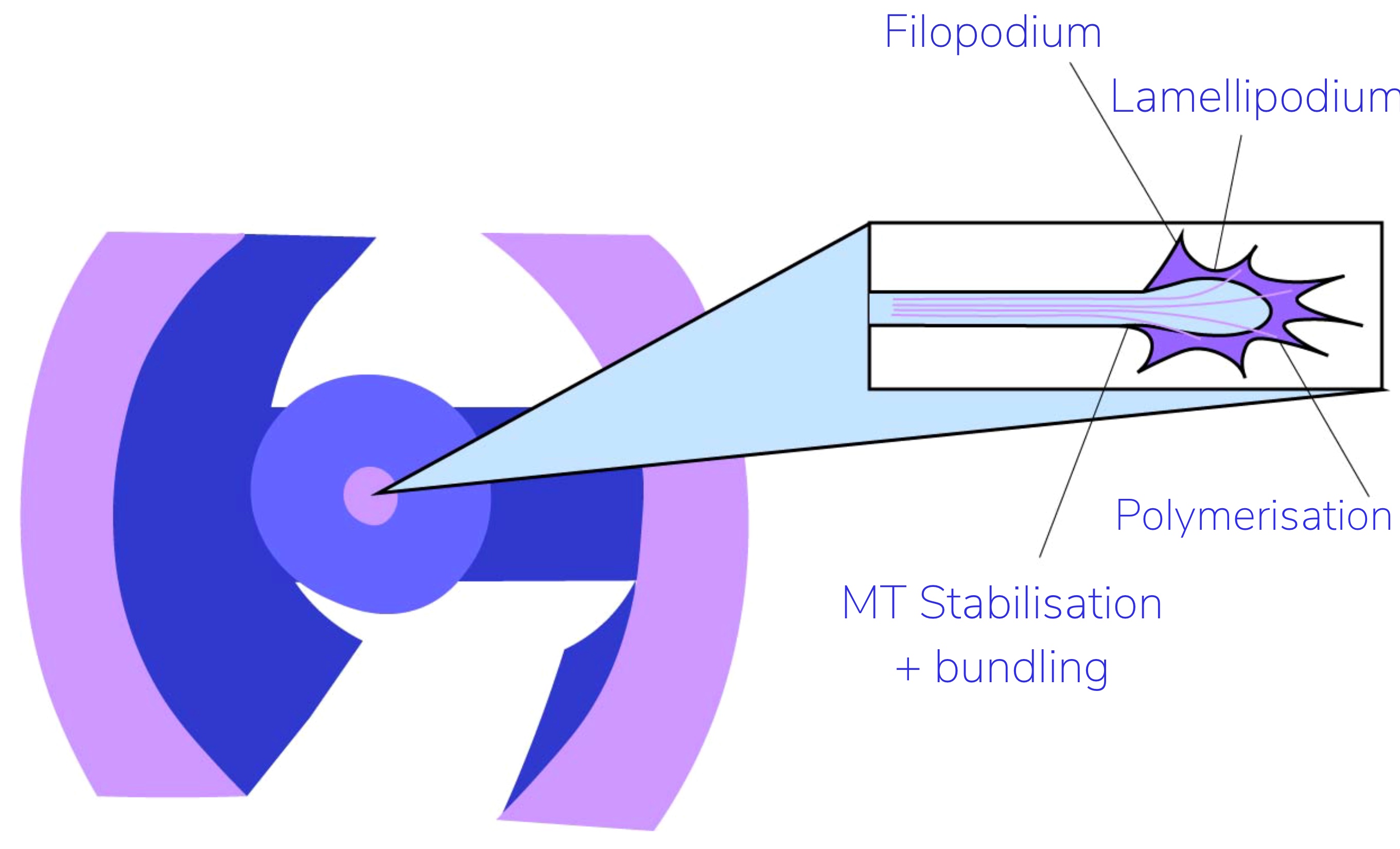
Competitors of ChABC: PP2A
Some studies show that treatment to enhance Protein phosphatase type 2A (PP2A) activity remarkably increases axon outgrowth and facilitates functional recovery after SCI. PP2A cleaves phosphate groups from serine and threonine residues. In this developing central nervous system (CNS), this phosphatase promotes axogenesis by dephosphorylating the cytoplasmic protein collapsin response mediator protein-2 (CRMP2). CRMP2 binds to α–β-tubulin dimers to promote microtubule polymerization and stabilization resulting in increased neurite outgrowth, which is normally inhibited by the majority of phosphorylations. In SCI, kinases which phosphorylate CRMP2 are overactived (Cheng et al., 2015).
In addition, within the syringomyelia, CNS inhibiting substrates, such as chondroitin sulfate proteoglycans (CSPGs) and myelin associated glycoproteins (MAG), are able to inactivate PP2A, preventing dephosphorylation of CRMP2. Treatment to increase PP2A activity promotes neurite outgrowth and counteracts the inhibitory effect of CSPGs and MAGs, creating a more permissive microenvironment in vitro. (Mimura et al., 2006; Nagai et al., 2016). However, research is still in its very early stages and the main limitation lies in the invasiveness of the in vivo mice model through the use of a subcutaneous osmotic pump that penetrates the dura mater to deliver DES.
Can ChABC treatment replace a biocompatible scaffold?
Non-surgical ChABC treatment does not yet have the potential to completely replace scaffold insertions; while ChABC treatment can aid in regeneration of lesioned axons, there is insufficient data on its effects on axon growth alignment - a metric for the ability of a surface to guide neuronal growth. Axon growth is highly random after injury, and rarely extends past the lesion site back into the host tissue - without the additional support of nerve guidance channels or scaffold structures, axons do not seem to migrate back towards their targets, even though their regrowth might be stimulated (Hoffman-Kim et al., 2010).
Overall, pre-clinical evidence suggests that ChABC treatment is less suitable for helping axonal regrowth where there are larger lesions accompanying severe SCI symptoms, although the studies were conducted on rate models of SCI. The data remains largely inconclusive for human subjects (Bradbury et al., 2002).
Evaluating Novel Approaches
The research described above has provided a foundation for the implementation of a non-surgical method of promoting axon regeneration post SCI. Our current research suggests that ChABC will be the most effective in promoting axonal regeneration because it has already been administered as an intraspinal injection in animals, supporting its non-surgical implementation. In contrast, PP2A has only been activated with an agonist using subcutaneous osmotic pumps. These pumps are placed over the cyst and pierce the dura, which is a much more invasive approach (Cheng et al., 2015).
After a careful consideration of the potential candidates for our treatment, the two strongest candidates for the treatment of SCI were identified as the scaffold design and the ChABC treatment. The scaffold demonstrated a promising ability in promoting axonal guidance through topology and topography, as well as performing well in targeting the chronic phase of SCI. The protease, on the other hand, offered a non-invasive option for the treatment of the chronic phase. Ultimately, we decided our scaffolding provided a more comprehensive treatment for larger cavities as it provides both mechanical support and promotes axonal regrowth at the site of the lesion. Our scaffold has mechanical properties that are adapted to match the tissue of the spinal cord (Hejčl et al., 2008) - the design includes pores that are shown to facilitate axonal outgrowth (Nisbet et al., 2008). Alongside our scaffold, adhesion molecules from our mussel foot protein can be used to enhance cell attachment and tissue growth. A biocompatible scaffold design also has the potential to incorporate growth promoting molecules and/or a drug delivery system (Hynd et al., 2007; Willerth and Sakiyama-Elbert, 2007). Overall, our scaffolding had clear advantages over the hydrogel and the most promising enzymatic candidate, Chondroitinase ABC.
Similarly, we considered the implication of different stem cells alongside our scaffold design - relative to our project design we decided that their application was most suited to the acute stage of spinal cord injuries. The collaborative effect of the scaffold and stem cells have a potential to prevent the growth of the glial scar in totality, which affirms its efficacy in the acute stage.

However, growth factors and other growth promoting molecules are still required to promote the growth of neurons and optimal growth conditions are still being investigated by researchers. Other limitations include some stem cells, such as neural stem cells and mesenchymal stem cells, have a preferential capability to differentiate into glial lineages and have low neuronal differentiation. This can promote astrogliosis, extending the glial scar and therefore resulting in poor recovery (Shrestha et al., 2014). Gene modification of these cells has shown some promising results, although the research remains in its primary stages.
Presently, our scaffold is designed to target the chronic stage, where the glial scar has fully formed and axonal ability to regenerate has been greatly reduced. Future investigations may include the deliberation of most appropriate stem cells and their capacity to improve neurological outcomes. In phase two of our project, we are considering the possibility of testing stem cells’ capacity to regenerate in the lab, pending the ethical approval. The table below discusses the differences between our current candidates:
Table 2: Comparing Neural Stem cells and Mesenchymal Stem Cells (Cofano et al., 2019; Shrestha et al., 2014).
| Neural stem cells (NSCs) | Mesenchymal stem cells (MSCs) | |
|---|---|---|
| Advantages | They promote neural differentiation and synaptogenesis in scaffoldings. | They can downregulate apoptotic and upregulate anti-apoptotic molecules, which prevents oligodendrocyte apoptosis-induced demyelination and axon degeneration in a post- SCI environment. They can also regulate the activation of macrophages at the site of an SCI. In addition, they pose a limited ethical concern and present a low risk of developing into a tumour. |
| Limitations | They can differentiate into glial cell lineages, particularly astrocytes.They have low neuronal differentiation. This can induce astrogliosis and extension of the glial scar resulting in poor functional recovery of an SCI patient. | Lack of neural differentiation, low survival rate of grafted cells, and a host immune response |
Utilising Synthetic Polymers
This year, we decided to specifically focus on the implementation of synthetic polymers alongside our scaffold design, instead of using a stem cell approach. However, synthetic polymers do not create an optimal environment for cell adhesion and would require an addition of a bioadhesive to fulfil this function. After evaluating a review paper on hydrogels, we discovered the rising potential in mussel foot proteins (MFP’s) for use as biological adhesives. The issue with current adhesives is that they do not maintain their adhesiveness in aqueous environments. Mussels, however, have evolved a way to maintain adhesiveness underwater in the form of MFP’s, highlighting their potential to be used within the body for sutureless surgeries, as well as reducing the need for metal pins to secure structures in place. Accordingly, integrating MFP into our scaffold has a potential to improve axonal ingrowth after implantation and effectively promote axon regeneration.
MFP’s contain catechol groups in the form of DOPA residues (3,4-dihydroxyphenylalanine), an adhesive molecule with a wide range of different bonding possibilities, which enables the mussel to bind to a variety of different surfaces. After researching into the properties of MFPs from a range of different species, we decided to look further into pvfp-5β. This MFP is the first to be secreted into the mussel foot in the formation of the mussel byssus in the asian green mussel (Perna viridis). It contains a high percentage of DOPA in comparison to other MFP’s, and adopts an unordered and elongated structure which maximises DOPA interactions with the contacting surface. As the mussel byssus gradually evolved to withstand turbulent tidal forces which bombard the surfaces in which mussels attach, the protein has also adapted and enhanced its adhesiveness (Santonocito et al., 2019). We hope that the incredible adhesive ability of pvfp-5β will ensure our adhesive is strong enough to keep our scaffold secure, especially as the spine is a very mobile part of the body. Many mussel foot proteins, including pvfp-5β, have been successfully synthesised in recombinant E. coli, providing a confirmed route into synthesising our MFP. We therefore identified this MFP as the ideal candidate for our adhesive.
After further investigations into Pvfp-5β, we found that MFP’s have been shown to elicit minimal immune responses within the body. The biocompatibility of MFP’s reduces the complications of the immune system damaging our scaffold, also reducing any unanticipated immunogenic complications. After contacting Dr. Koffler, we discovered that the scaffold must maintain structurally sound for at least 6 months to ensure suitable recovery has taken place for the body to continue to repair once the scaffold degrades. Coating our scaffold with a bioadhesive MFP polymer thereby has a potential to reduce the rate of scaffold degradation and negate the need for immunosuppressant therapy.
References:
- Alizadeh, A., Dyck, S.M., Karimi-Abdolrezaee, S., 2019. Traumatic Spinal Cord Injury: An Overview of Pathophysiology, Models and Acute Injury Mechanisms. Front. Neurol. 10, 282. https://doi.org/10.3389/fneur.2019.00282
- Bartus, K., James, N.D., Didangelos, A., Bosch, K.D., Verhaagen, J., Yáñez-Muñoz, R.J., Rogers, J.H., Schneider, B.L., Muir, E.M., Bradbury, E.J., 2014. Large-Scale Chondroitin Sulfate Proteoglycan Digestion with Chondroitinase Gene Therapy Leads to Reduced Pathology and Modulates Macrophage Phenotype following Spinal Cord Contusion Injury. J. Neurosci. 34, 4822–4836. https://doi.org/10.1523/JNEUROSCI.4369-13.2014
- Batzdorf, U., 1991. A Brief History of Syringomyelia, in: Tamaki, N., Batzdorf, U., Nagashima, T. (Eds.), Syringomyelia. Springer Japan, Tokyo, pp. 3–9. https://doi.org/10.1007/978-4-431-67893-9_1
- Bradbury, E.J., Moon, L.D.F., Popat, R.J., King, V.R., Bennett, G.S., Patel, P.N., Fawcett, J.W., McMahon, S.B., 2002. Chondroitinase ABC promotes functional recovery after spinal cord injury. Nature 416, 636–640. https://doi.org/10.1038/416636a
- Bradbury, E.J., Carter, L.M., 2011. Manipulating the glial scar: Chondroitinase ABC as a therapy for spinal cord injury. Brain Research Bulletin 84, 306–316. https://doi.org/10.1016/j.brainresbull.2010.06.015
- Brodbelt, A.R., Stoodley, M.A., 2003. Post-traumatic syringomyelia: a review. Journal of Clinical Neuroscience 10, 401–408. https://doi.org/10.1016/S0967-5868(02)00326-0
- Burda, J.E., Sofroniew, M.V., 2014. Reactive Gliosis and the Multicellular Response to CNS Damage and Disease. Neuron 81, 229–248. https://doi.org/10.1016/j.neuron.2013.12.034.
- Burke, M.A., Yip, S.T., 2017. (74) Attorney, Agent, or Firm — Idea Intellectual Limited; 22.
- Chau, C.H., Shum, D.K.Y., Li, H., Pei, J., Lui, Y.Y., Wirthlin, L., Chan, Y.S., Xu, X. ‐M., 2004. Chondroitinase ABC enhances axonal regrowth through Schwann cell‐seeded guidance channels after spinal cord injury. FASEB j. 18, 194–196. https://doi.org/10.1096/fj.03-0196fje
- Cheng, P., Chen, K., Yu, W., Gao, S., Hu, S., Sun, X., Huang, H., 2015. Protein phosphatase 2A (PP2A) activation promotes axonal growth and recovery in the CNS. Journal of the Neurological Sciences 359, 48–56. https://doi.org/10.1016/j.jns.2015.10.025
- Cofano, F., Boido, M., Monticelli, M., Zenga, F., Ducati, A., Vercelli, A., Garbossa, D., 2019. Mesenchymal Stem Cells for Spinal Cord Injury: Current Options, Limitations, and Future of Cell Therapy. IJMS 20, 2698. https://doi.org/10.3390/ijms20112698
- Day, P., Alves, N., Daniell, E., Dasgupta, D., Ogborne, R., Steeper, A., Raza, M., Ellis, C., Fawcett, J., Keynes, R., Muir, E., 2020. Targeting chondroitinase ABC to axons enhances the ability of chondroitinase to promote neurite outgrowth and sprouting. PLoS ONE 15, e0221851. https://doi.org/10.1371/journal.pone.0221851
- Elliott, N.S.J., 2009. Mathematical Modelling and Analysis of Cerebrospinal Mechanics: An Investigation Into the Pathogenesis of Syringomyelia 255.
- Fan, B., Wei, Z., Yao, X., Shi, G., Cheng, X., Zhou, X., Zhou, H., Ning, G., Kong, X., Feng, S., 2018. Microenvironment Imbalance of Spinal Cord Injury. Cell Transplant 27, 853–866. https://doi.org/10.1177/0963689718755778
- Hédoux, A., Willart, J.-F., Paccou, L., Guinet, Y., Affouard, F., Lerbret, A., Descamps, M., 2009. Thermostabilization Mechanism of Bovine Serum Albumin by Trehalose. J. Phys. Chem. B 113, 6119–6126. https://doi.org/10.1021/jp900330r
- Heiss, J.D., Snyder, K., Peterson, M.M., Patronas, N.J., Butman, J.A., Smith, R.K., DeVroom, H.L., Sansur, C.A., Eskioglu, E., Kammerer, W.A., Oldfield, E.H., 2012. Pathophysiology of primary spinal syringomyelia: Clinical article. SPI 17, 367–380. https://doi.org/10.3171/2012.8.SPINE111059
- Hejčl, A., Lesný, P., Štulík, J., Syková, E., 2008. Biocompatible Hydrogels in Spinal Cord Injury Repair 57, 12.
- Hoffman-Kim, D., Mitchel, J.A., Bellamkonda, R.V., 2010. Topography, Cell Response, and Nerve Regeneration. Annu. Rev. Biomed. Eng. 12, 203–231. https://doi.org/10.1146/annurev-bioeng-070909-105351
- Hong, L.T.A., Kim, Y.-M., Park, H.H., Hwang, D.H., Cui, Y., Lee, E.M., Yahn, S., Lee, J.K., Song, S.-C., Kim, B.G., 2017. An injectable hydrogel enhances tissue repair after spinal cord injury by promoting extracellular matrix remodeling. Nat Commun 8, 533. https://doi.org/10.1038/s41467-017-00583-8
- Hoque, M., Yong, L. and Ian, P. (2012) ‘MATHEMATICAL MODELING ON DEGRADATION OF 3D TISSUE ENGINEERING SCAFFOLD MATERIALS’, Official Journal of Tissue Engineering and Regenerative Medicine Society of Malaysia, 1(1), pp. 58–61.
- Huebner, E.A., Strittmatter, S.M., 2009. Axon Regeneration in the Peripheral and Central Nervous Systems, in: Koenig, E. (Ed.), Cell Biology of the Axon, Results and Problems in Cell Differentiation. Springer Berlin Heidelberg, Berlin, Heidelberg, pp. 305–360. https://doi.org/10.1007/400_2009_19
- Hynd, M.R., Turner, J.N., Shain, W., 2007. Applications of hydrogels for neural cell engineering. Journal of Biomaterials Science, Polymer Edition 18, 1223–1244. https://doi.org/10.1163/156856207782177909
- Kirshblum, S.C., Burns, S.P., Biering-Sorensen, F., Donovan, W., Graves, D.E., Jha, A., Johansen, M., Jones, L., Krassioukov, A., Mulcahey, M.J., Schmidt-Read, M., Waring, W., 2011. International standards for neurological classification of spinal cord injury (Revised 2011). The Journal of Spinal Cord Medicine 34, 535–546. https://doi.org/10.1179/204577211X13207446293695
- Lee, H., McKeon, R.J., Bellamkonda, R.V., 2010. Sustained delivery of thermostabilized chABC enhances axonal sprouting and functional recovery after spinal cord injury. Proc Natl Acad Sci USA 107, 3340–3345. https://doi.org/10.1073/pnas.0905437106
- Mimura, F., Yamagishi, S., Arimura, N., Fujitani, M., Kubo, T., Kaibuchi, K., Yamashita, T., 2006. Myelin-associated Glycoprotein Inhibits Microtubule Assembly by a Rho-kinase-dependent Mechanism. J. Biol. Chem. 281, 15970–15979. https://doi.org/10.1074/jbc.M510934200
- Nagai, J., Owada, K., Kitamura, Y., Goshima, Y., Ohshima, T., 2016. Inhibition of CRMP2 phosphorylation repairs CNS by regulating neurotrophic and inhibitory responses. Experimental Neurology 277, 283–295. https://doi.org/10.1016/j.expneurol.2016.01.015
- Nisbet, D.R., Crompton, K.E., Horne, M.K., Finkelstein, D.I., Forsythe, J.S., 2008. Neural tissue engineering of the CNS using hydrogels. J. Biomed. Mater. Res. 87B, 251–263. https://doi.org/10.1002/jbm.b.31000
- Patek, M., Stewart, M., 2020. Spinal cord injury. Anaesth. Intensive Care Med. 21, 411–416. https://doi.org/10.1016/j.mpaic.2020.05.006
- Rai, S.K.R., Rai, P.S.K., 2015. Volume change theory for syringomyelia: A new perspective.
- Rasouli, A., Bhatia, N., Dinh, P., Cahill, K., Suryadevara, S., Gupta, R., 2009. Resection of glial scar following spinal cord injury. J. Orthop. Res. 27, 931–936. https://doi.org/10.1002/jor.20793
- Rath, N., Balain, B., 2017. Spinal cord injury—The role of surgical treatment for neurological improvement. Journal of Clinical Orthopaedics and Trauma 8, 99–102. https://doi.org/10.1016/j.jcot.2017.06.016
- Santonocito, R., Venturella, F., Dal Piaz, F., Morando, M.A., Provenzano, A., Rao, E., Costa, M.A., Bulone, D., San Biagio, P.L., Giacomazza, D., Sicorello, A., Alfano, C., Passantino, R., Pastore, A., 2019. Recombinant mussel protein Pvfp-5β: A potential tissue bioadhesive. J. Biol. Chem. 294, 12826–12835. https://doi.org/10.1074/jbc.RA119.009531
- Shrestha, B., Coykendall, K., Li, Y., Moon, A., Priyadarshani, P., Yao, L., 2014. Repair of injured spinal cord using biomaterial scaffolds and stem cells. Stem Cell Res Ther 5, 91. https://doi.org/10.1186/scrt480
- Tsintou, M., Dalamagkas, K., Seifalian, A.M., 2015. Advances in regenerative therapies for spinal cord injury: a biomaterials approach. Neural Regen. Res. 10, 726–742. https://doi.org/10.4103/1673-5374.156966.
- Wang, P., Wang, H., Ma, K., Wang, S., Yang, C., Mu, N., Yang, F., Feng, H., Chen, T., 2020. Novel cytokine-loaded PCL-PEG scaffold composites for spinal cord injury repair. RSC Adv. 10, 6306–6314. https://doi.org/10.1039/C9RA10385F
- Warden, P., Bamber, N.I., Li, H., Esposito, A., Ahmad, K.A., Hsu, C.Y., Xu, X.M., 2001. Delayed Glial Cell Death Following Wallerian Degeneration in White Matter Tracts after Spinal Cord Dorsal Column Cordotomy in Adult Rats. Experimental Neurology 168, 213–224. https://doi.org/10.1006/exnr.2000.7622
- Waters, R.L., Adkins, R.H., Yakura, J.S., 1991. Definition of complete spinal cord injury. Spinal Cord 29, 573–581. https://doi.org/10.1038/sc.1991.85
- Willerth, S.M., Sakiyama-Elbert, S.E., 2007. Approaches to neural tissue engineering using scaffolds for drug delivery. Advanced Drug Delivery Reviews 59, 325–338. https://doi.org/10.1016/j.addr.2007.03.014
- Woolf, C.J., Salter, M.W., 2000. Neuronal Plasticity: Increasing the Gain in Pain. Science 288, 1765–1768. https://doi.org/10.1126/science.288.5472.1765
- Zhang, N., Yin, Y., Xu, S.-J., Wu, Y.-P., Chen, W.-S., 2012. Inflammation & apoptosis in spinal cord injury. INDIAN J MED RES 11.
- Zhu, W., Zhang, H., Chen, X., Jin, K., Ning, L., 2018. Numerical characterization of regenerative axons growing along a spherical multifunctional scaffold after spinal cord injury. PLoS ONE 13, e0205961. https://doi.org/10.1371/journal.pone.0205961










